Wellington Eye Centre’s Ophthalmologist
If you have any problems with lost vision in one or both eyes, it’s important to get your eyes checked as soon as possible. However, it is quite normal to be living with an eye condition at some point of your life. Some are more debilitating than others, and some have an easy fix. Different eye conditions can be brought on by a number of factors such as age, illnesses, exposure to irritants and trauma. We’re going to cover some of the most common eye conditions in New Zealand. Read our article about common age-related eye conditions if you’d like to learn more about eyesight when you age.
So, what are the most common eye conditions in NZ for people of all ages?
Diabetic retinopathy
Retinopathy is the medical term for disease of the retina. It is the leading cause of loss of vision in people between the ages of 20 and 65. Damage to the retina from retinopathy can have a significant impact on vision.
Causes of Diabetic Retinopathy
Diabetic retinopathy, also known as diabetic eye disease, occurs in people who have type one diabetes or type two diabetes. It occurs because of the biochemical changes in the blood due to diabetes, which causes damaged blood vessels in the retina, and can lead to severe loss of vision if untreated. Up to 80% of people who have had diabetes for more than 20 years will develop diabetic retinopathy. The longer the person has diabetes, the greater the chance that they will develop diabetic retinopathy.
If untreated, diabetic retinopathy usually steadily progresses. In its early stages, known as non-proliferative diabetic retinopathy, vision may be completely normal. The only way to detect early non-proliferative retinopathy is to have an eye examination by an ophthalmologist or optometrist. With progression, abnormal blood vessels develop at the back of the eye. This is known as proliferation. These abnormal blood vessels can bleed, leak fluid into the retina (known as oedema) or cause scarring and can eventually cause severe and irreparable loss of vision.
Macular oedema is the term used to describe leakage of fluid into the centre of the retina from abnormal, leaky blood vessels. This can occur at any stage of diabetic retinopathy and can cause significant damage to central vision.
Risk factors for people with Diabetic Retinopathy
There are several risk factors associated with the development of diabetic retinopathy. It becomes more common the longer a person has had diabetes, poor control of blood sugar and diabetes, and it’s more likely to progress during pregnancy. Because early diabetic retinopathy may have no effect on vision, a person with diabetes may not be aware of any problems with their vision until the retinopathy has progressed to an advanced stage. For this reason, anybody who has diabetes must have regular eye checks, even if they have normal vision. Pregnant women with diabetes should have their eyes checked every three months during pregnancy. In New Zealand, free diabetic eye screening using retinal cameras is available, this is usually organised by family doctors.
Treatment for Diabetic Retinopathy
A number of treatments are available for treating diabetic retinopathy, but these are more effective if they are used before the condition becomes advanced. This reiterates the importance of having regular eye examinations, so that treatment can be provided before the condition becomes too severe.
Treatments include laser treatment to close off abnormal blood vessels and injections of medications which do the same thing. It’s important to manage diabetes so that blood sugar levels remain within normal limits as this has been shown to reduce the development and progression of diabetic retinopathy.
Dry eyes
The term “dry eyes” refers to the condition where the eyes are inadequately lubricated by the normal tears that are produced by the tear glands. This can occur if the tear glands do not produce enough tears to keep the eyes wet (known as secretory dry eyes), or if the tears being produced evaporate more rapidly than they can be replaced on the surface of the eye (known as evaporative dry eyes).
Symptoms of Dry Eyes
An adequate tear film is important to maintain normal vision and to maintain a healthy surface on the eye. Symptoms of dry eyes can include stinging, grittiness, light sensitivity, a foreign body sensation, blurred vision or tired eyes, difficulty wearing contact lenses and even watery eyes can be a symptom of dry eyes. Watery eyes can occur because the body responds to the irritation caused by dry eyes by increasing tear production.
In many cases someone with dry eyes may have both evaporative and secretory dry eyes and have multiple causes for their problem.
Causes of secretory dry eyes:
- Ageing
- Medical conditions including rheumatoid arthritis or lupus thyroid disorders and diabetes
- Medications including antihistamines and decongestants, antidepressants, some drugs used to treat high blood pressure, acne medications, some contraceptives and medications used to treat Parkinson’s disease
- Following laser eye surgery (this is usually temporary)
Causes of evaporative dry eyes include:
- Exposure to wind, smoke, or dry air from air conditioning heat pumps or air travel
- Reduced blink rate which typically occurs with visual tasks requiring concentration, such as reading, working on a computer or driving
- A very common cause of evaporative dry eyes is an abnormality of the oil glands (meibomian glands) found on the edge of the eyelids. These glands usually produce an oil which floats onto the tear film and prevents the tears evaporating when the eyes are open. When there is an abnormality in them it means that the oil produced is insufficient, which in turn, causes the tears to evaporate faster
Treatments for Dry Eye
There are several treatments for dry eye which can be very effective, and most people who suffer from dry eyes can have their symptoms significantly reduced with adequate treatment.
Artificial tears
Artificial tears are used to supplement the natural tears produced by the tear glands and can be bought over the counter at most pharmacies and supermarkets. Some people with severe dry eyes can receive a subsidy from the government towards the cost of artificial tears.
Dietary supplements
Omega three dietary supplements are very beneficial for the treatment of dry eyes, particularly evaporative dry eyes. It’s important to note that these are not a cure and may need to be taken long-term.
Drinking lots of water
Adequate hydration is important in the management of dry eyes. If you suffer from dry eyes you should make sure that you drink a lot of fresh water.
Intense Pulsed Light Therapy
Intense pulsed light therapy (IPL) can be very useful in improving the functioning of the oil glands in the eyelids. This is particularly useful for evaporative dry eye treatment and is available from many ophthalmologists or optometrists.
Restasis
A medicated eye drop called Restasis has been shown to increase tear production by reducing inflammation in the tear glands and on the surface of the eye. This can be especially useful in secretory dry eyes. Restasis is not available on prescription in New Zealand but can be prescribed by an ophthalmologist.
If you think that you could be suffering from dry eye syndrome you should have an eye check with an ophthalmologist or optometrist to correctly diagnose the condition and start the appropriate treatment.
Keratoconus
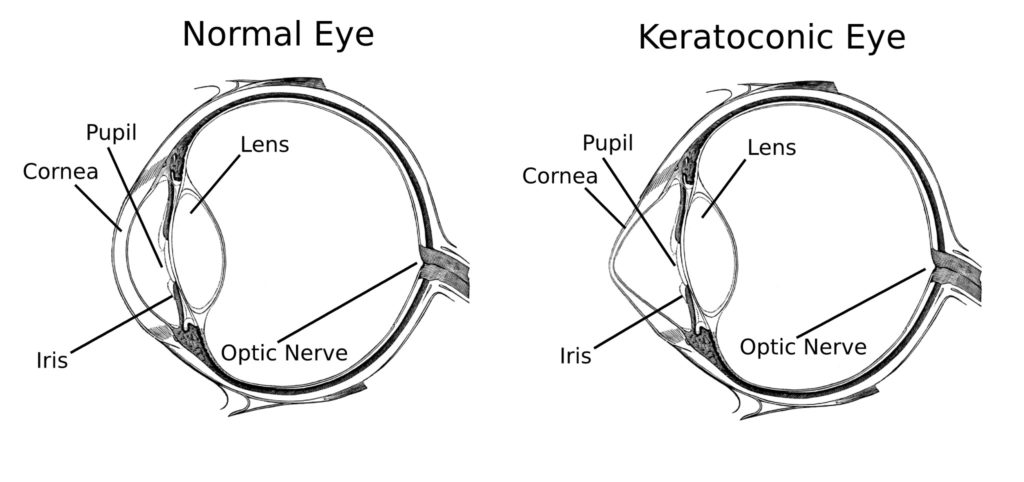
Keratoconus is a condition which causes distortion and bulging of the cornea of the eye. The cornea is the clear, lens shaped structure which sits in front of the iris (the coloured part of the eye). The cornea is responsible for about 60% of the total focusing power of the eye and can only carry out its function properly if it is evenly curved in all directions.
Keratoconus usually develops in preteen or teenage years and can progress rapidly in young people if it’s not treated. The condition is very common in New Zealand and it’s thought that many young people may have the condition and be undiagnosed. Keratoconus is a serious eye condition and can have lifelong consequences for education, career choices and sporting activities.
Causes of Keratoconus
Keratoconus causes distortion of the shape of the cornea, and can cause severe impairment of vision, which may not be able to be corrected by glasses or contact lenses. Kerataconus can also cause double vision and an increase in glare.
Keratoconus can run in families, but it’s most commonly associated with allergic conditions such as hay fever, asthma and eczema. It’s thought that keratoconus occurs in young people with allergies because of chronic eye rubbing caused by itchy eyes. Eye rubbing is thought to cause inflammation in the cornea and damage to the connective tissue which makes up the bulk of the cornea. As a result, the connective tissue becomes weak and the cornea is no longer able to support the pressure inside the eye and starts to bulge. This bulging will usually progress in young people, resulting in progressive deterioration and vision.
Eventually someone with keratoconus may only achieve adequate vision by wearing hard contact lenses and may eventually need a corneal transplant. It’s the most common cause of corneal transplantation in New Zealand and most other countries in the developed world. Fortunately, there are a number of things that can be done to prevent or halt the progression of the condition.

Treatments for Keratoconus
Keratoconus is a progressive condition affecting young people and can cause lifetime impairment of vision. It’s able to be treated to prevent ongoing deterioration and therefore it’s vital that keratoconus is detected as soon as possible. If a young person is experiencing deteriorating vision, especially if they have itchy eyes or rub their eyes, they should have their eyes checked by an ophthalmologist or optometrist to detect any signs of keratoconus so that appropriate treatment can be carried out.
Any young person who rubs their eyes regularly should be strongly discouraged from doing so. If they suffer from allergies such as hay fever and get itchy eyes, they should see an ophthalmologist or optometrist for medications to control the itching. There is also a medical treatment available that has been shown to be very effective at halting the progression of keratoconus. This treatment is called Corneal Collagen Cross-Linking. This treatment is available at most public hospital eye outpatient clinics in New Zealand and is also available at many private specialist ophthalmologist clinics. Most health insurance companies will cover the cost of cross-linking if the keratoconus is progressing.
Pterygium
A pterygium is a growth of tissue which spreads on to the cornea from the white of the eye (conjunctiva). They usually occur on the side of the eye closest to the nose and have a triangular shape. A pterygium can be thought of as being a bit like scar tissue. They are not cancerous and have no effects on health apart from immediate effects on the eye and vision.
A pterygium can remain quite small and cause no symptoms, or may get progressively bigger over time, extending towards the centre of the cornea. If a pterygium is thickened or becomes extensive, it can cause significant symptoms, including redness, irritation and discomfort, distortion of vision, and if it is large enough can even cause significant visual loss.
What causes Pterygiums
The cause of pterygiums is not fully understood. However, exposure to ultraviolet light is thought to be a major causing factor because pterygiums are more common in tropical or dry climates with high ultraviolet light levels and are more common in people who work outdoors or exposed to increased levels of sunlight. Because of this it is commonly referred to as “Surfer’s Eye”. They are significantly more likely to occur in men than in women, and are very uncommon in children. Genetic factors may have some effect on the development of pterygiums because they have a tendency to run in families.
A small pterygium that is not affecting vision or causing any symptoms can safely be left alone without removal. However, it should be checked periodically to make sure that it is not getting bigger and posing a risk to vision.
Reasons for removing a pterygium include:
- A pterygium that’s causing an alteration or deterioration in vision. Or if its getting bigger and is starting to affect vision.
- If it is causing irritation, discomfort or redness. A pterygium that is thickened may cause significant redness and discomfort. Particularly if the eye is exposed to irritants such as smoke, or a dry or dusty atmosphere.
- If it is causing cosmetic issues.
- If it interferes with being able to wear contact lenses. Because a pterygium extends onto the cornea, it can impact the ability to wear soft or hard contact lenses. A pterygium can also prevent laser eye surgery, such as SMILE ® or LASIK, being performed. In some cases the removal of a pterygium may allow laser eye surgery to be carried out.
Pterygium removal is normally carried out using a local anaesthetic. The operation normally takes 15 to 30 minutes and does not require an overnight stay in a hospital. The pterygium is carefully peeled off the cornea and the scarred tissue is removed. This leaves a bare surface at the site of the pterygium which is usually covered with a graft of tissue from elsewhere on the surface of the eye. This graft speeds healing following surgery and reduces discomfort. It also reduces the chance of the pterygium re-occurring, which can happen in up to 20% to 30% of cases. Following the surgery, steroid and antibiotic eye drops may be used for several weeks.
So there you have it – some of the most common eye conditions in New Zealand. Feel free to get in touch with the team at Wellington Eye Centre if you have any other questions or wish to book a consultation with Dr Logan. You can call us on 0800 733 327 or complete the contact form below.
SMILE ® is a registered trademark of Carl Zeiss Meditec.

Festive Season and Your Eyes

Vitamins For Good Eye Health and Vision

Help my eyelid is twitching!

Do you need to have eye exams after laser eye surgery?

Restasis Eye Drops for the Treatment of Dry Eyes

Meet The Team at the Wellington Eye Centre

Festive Season and Your Eyes

Naumi Studio Hotel Wellington

What to Expect on The Day of Surgery