Laser eye surgery is more popular now than ever. Once you’ve made the first step of deciding to proceed with the surgery, you need to start thinking about preparation. It is a quick and safe procedure, but even the smallest operations require some planning. Something as simple as asking someone to drive you home in advance will help to make the experience as smooth and carefree as possible. Our team of experts at Wellington Eye Centre have compiled a comprehensive list of tips for getting procedure ready. So, let’s dive in!
How does laser eye surgery work?
All laser eye surgery procedures (LASIK, SMILEⓇ or PRK) work by doing the same thing. They reshape the cornea, which is the clear dome part at the front of your eye. By reshaping the cornea, we are able to adjust where the eyes focal point is so it sits neatly on the back of the eye, giving a clear image. The way the focal point needs to be adjusted will depend on whether you are short-sighted or long-sighted. For short-sighted people, the cornea will need to be flattened to reduce the refractive power. This is due to the cornea being too curved, or the eye being too long. Whilst for long-sighted people, the cornea is steepened to increase the refractive power; as the cornea is too flat or the eye is too short.
Considering laser eye surgery? Here’s how to get started:
The first step is to make an appointment for a free laser assessment. At this appointment, we will do a number of scans and tests on your eyes, talk to you about your medical history, check your vision and discuss the different types of surgery. This assessment is with one of our friendly ophthalmic technicians and takes around an hour.
Before you book your laser eye surgery assessment
For those who love doing research, we’ve written down a list of information that is helpful to collect for your surgeon, along with some top tips for getting ready for your surgery. Most of this will also be covered during your free laser surgery suitability assessment or during subsequent appointments.
1. A list of your current medications
This is important as some medications alter how your body responds to surgery and can cause:
- excess inflammation.
- dry your eyes out, potentially making the healing process more challenging for you.
- affect your vision, possibly resulting in an inaccurate vision test
These medications probably won’t rule laser vision correction out for you, but may mean your surgeon needs to counter the effects of these medications. This can be as simple as changing the eye drops they prescribe after surgery.
2. Family medical history – do you or your family members have any history of eye disease or autoimmune conditions?
We are especially interested in the following eye diseases:
- Keratoconus – a condition that can mean a person wears hard contact lenses (rigid contact lenses) or may have had a corneal graft.
- Glaucoma – a condition that involves increased pressure inside the eye, often treated with eye drops, sometimes with surgery.
We will also ask about the systemic conditions below:
- Autoimmune conditions like rheumatoid arthritis or lupus; as these autoimmune conditions can exacerbate the inflammatory response to surgery, making the healing process unpredictable.
- A history of herpes simplex (cold sores) or herpes zoster (shingles). If these conditions have affected the eyes, the cornea may already be compromised with reduced sensitivity. In the case of herpes simplex, surgery could trigger a recurrence of this infection.
- Diabetes, Type 1, Type 2 or gestational diabetes. Or even if you’re not being treated for diabetes, but perhaps you are being monitored by your GP due to elevated blood sugars. Sometimes it might be described as ‘borderline diabetes’. Some stages of diabetes can result in delayed healing so it helps if you can come to your appointment knowing about your current blood sugar control, your medications and recent Hba1c results.
3. Evidence of a stable spectacle prescription
If you can, ask your Optometrist for a summary of your spectacle refraction from the past few years and bring it along. Even if you don’t currently wear prescription spectacles, the results from your most recent Optometrist appointments can be really helpful in determining if your eyesight is changing regularly and by how much.
A small amount of variation in your spectacle prescription will not prevent you from having laser vision correction. But a consistent progressive change or unstable fluctuations in vision might affect your eligibility for the procedure.
The natural change in vision we experience over the age of forty years, called presbyopia, also won’t affect your suitability for laser vision correction. It may, however, alter which type of laser vision correction you are most suited to. Presbyopia is the gradual change in how we focus or accommodate objects up close.
4. Trial monovision contact lenses with your Optometrist.
This one is for patients 39 years or older who wear contact lenses.
Monovision is a style of visual correction that corrects one eye for distance vision. The other eye (usually the non-dominant eye) is used for tasks at distances of 30-50cm. This can be a helpful way to resolve the issues around needing one correction for distance and one for near.
With monovision, the eye that sees well for distance vision will be slightly blurred up close and the eye that sees well up close will be slightly blurred when looking at distant objects. But with both eyes open, typically the result is acceptably clear and comfortable vision at most distances.
As our need for reading spectacles increases after the age of 40 years, anyone coming in for a free laser assessment who is 39 years or older might have their suitability tested for monovision. If you want to trial monovision before your free assessment, check in with your Optometrist.
Nowadays, we prefer to perform LASIK Presbyond which is a surgical technique that can allow you to have blended vision, not monovision. However, trialling monovision contact lenses is a good test to see if you would be suitable for the more elegant form, blended vision. There are no contact lenses that mimic blended vision adequately.
5. Consider taking Omega 3 supplements.
It might be worth starting Omega 3 supplements. There is significant evidence that dietary supplements containing omega-3 oils are beneficial for the management of dry eye symptoms. These supplements can either be animal-based, sourced from krill, salmon or other fish oils, or vegetable-based, sourced from plant-based options like flaxseed oil. Anyone who suffers from dry eye symptoms should consider taking an omega-3 supplement. This should be in addition to using artificial tears and other measures for the management of the condition.
Dry eye is very common in contact lens wearers, adults over 60 years of age and women.
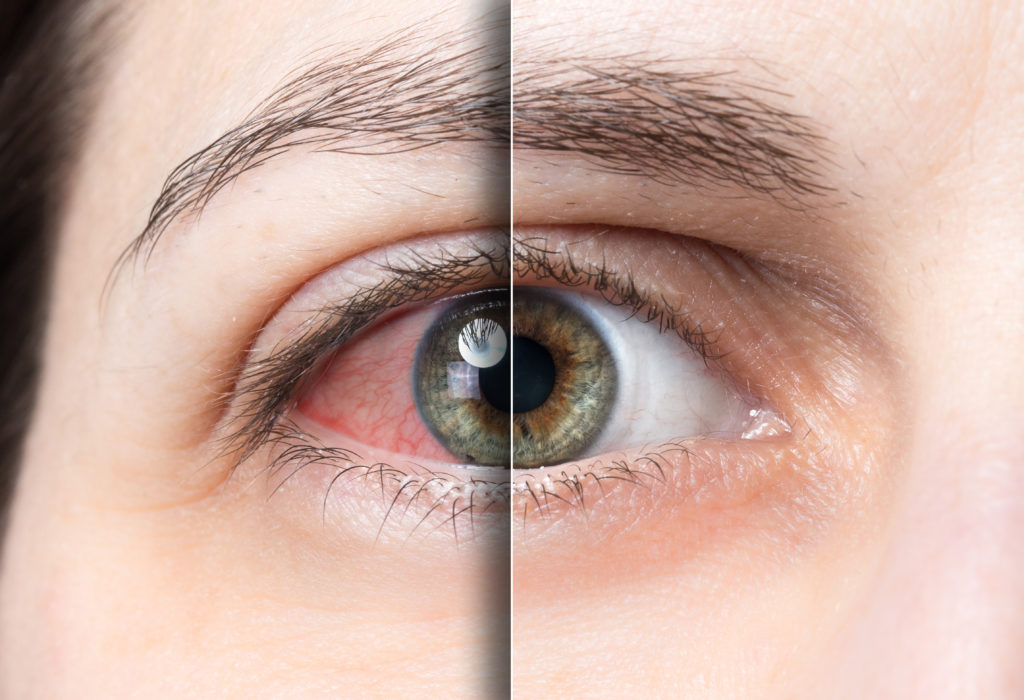
Since dry eyes are a common side effect of laser vision correction, especially in the first 6 months, it is often recommended that a person start Omega supplements before their surgery. If you have eyes prone to dryness, they are more likely to be dry immediately after the surgery. Treating even small amounts of corneal dryness before surgery is a great idea! There are also many other vitamins which are good for eye health – we even wrote a whole article about them!
6. Treat irritated eyes
If you have ever been diagnosed with hay fever, blepharitis or any other inflammatory eye conditions, make sure they are under control.
An eye that is inflamed before surgery will likely be more inflamed after surgery, more so than an eye that was calm and quiet before surgery. For this reason, we often treat a person’s hay fever or blepharitis before they have laser vision correction surgery. This might mean a few days or a few months of treatment before your surgery date can be arranged. Getting any irritation under control in advance is very helpful!
For those who suffer from seasonal allergies, it might be best to schedule your surgery for a time when your hay fever is less bothersome.
In the lead-up to laser eye surgery
You will be given specific pre-operative instructions to follow when you book surgery. Here are some things that will also be helpful to keep in mind:
- Read your consent form and surgery documents. It’s important that you read these and give us a call if you have any questions!
- For those who wear soft contact lenses, you cannot wear them for at least 5 days prior to the day of surgery.
- Don’t put anything on your face for 3 days prior to your procedure – no makeup, lotions, perfume etc. If you arrive with makeup on, we cannot do surgery.
- Take two panadol about an hour before you arrive – this helps for when the anaesthetic starts to wear off.
Preparing for recovery
Here are some helpful tips to set you up for a smooth recovery:
- Wear comfortable clothing! You will be laying down in theatre for 20-30 minutes and you don’t want to be uncomfortable.
- Organise for someone to drive you home. Although you will still be able to see and function, your vision will not be up to standard for driving or catching public transport.
- Rest your eyes! Make sure you have things ready to listen to – audiobooks, podcasts or music.
- Organise time off work. This can be 2-7 days after the day of surgery, depending on which type of surgery you have.
Remember, everyone’s recovery is slightly different. If you have any questions, please let us know. We’re here to help you every step of the way!
If you want to learn more about laser eye surgery then check out these articles written by our Ophthalmologist Dr Andrew Logan and our Optometrist Shannon Tubman:
- How Much Does Laser Eye Surgery Cost
- Risks and Complications of Laser Eye Surgery
- Laser Eye Surgery for Sports
- The Truth Behind Common Laser Eye Surgery Myths
If you have any other questions, get in touch – the team would love to help. You can also come in for a free laser suitability assessment, where our technician can answer any questions you may have.
SMILE® is a registered trademark of Carl Zeiss Meditec.

What to Expect on The Day of Surgery

What happens when your vision after laser vision correction surgery is not what you expected?

Am I too old to have laser eye surgery?

Dr Andrew Logans Innovation Achievements

Laser Eye Surgery for Sports

Meet The Team at the Wellington Eye Centre

Festive Season and Your Eyes

Naumi Studio Hotel Wellington

What to Expect on The Day of Surgery